Ozdikenosis is a rare and severe genetic disorder that progressively breaks down the body’s vital systems. Unlike more common illnesses, it remains poorly understood, but ongoing research is beginning to shed light on its devastating effects. This article provides a comprehensive overview of the disease, from its core mechanisms to the challenges of diagnosis and the search for a cure.
Key Takeaways
- Ozdikenosis is a rare, universally fatal genetic disorder that attacks the body’s cells, causing them to lose their ability to produce energy.
- The disease leads to a breakdown of vital organs, neurological functions, and the immune system.
- Early symptoms are often non-specific, leading to delayed diagnosis, which can be confirmed through a combination of clinical signs, imaging, and genetic testing.
- The disease progresses through three distinct stages, from subtle metabolic changes to complete multi-organ failure.
- There is currently no cure, and treatment focuses on managing symptoms and slowing the disease’s progression.
- Future hope lies in promising new research areas like gene therapy and stem cell treatments.
What Is Ozdikenosis?
Ozdikenosis is a rare, inherited medical condition where the body’s cellular energy systems fail. The name itself is not widely known, reflecting its low prevalence and the limited scientific literature available. It is considered a progressive multi-system disorder because it simultaneously affects multiple organ systems, which is one of the primary reasons it is so difficult to treat and manage.
The Discovery and Rarity of the Disease
The disease was first identified in the early 1980s by a team of researchers who observed a consistent pattern of unexplained organ failure in a small number of patients. Unlike widespread conditions, Ozdikenosis is thought to affect only about 1 in every 500,000 people globally, with a higher incidence in certain family lines due to its genetic nature. Its rarity has historically made it challenging to study, leading to significant delays in diagnosis and a lack of public awareness.
Why Does Ozdikenosis Kill You? The Pathophysiology
The fatal nature of Ozdikenosis lies in its comprehensive attack on the body’s most fundamental processes. It does not target a single organ; instead, it creates a systemic collapse that the body cannot recover from.
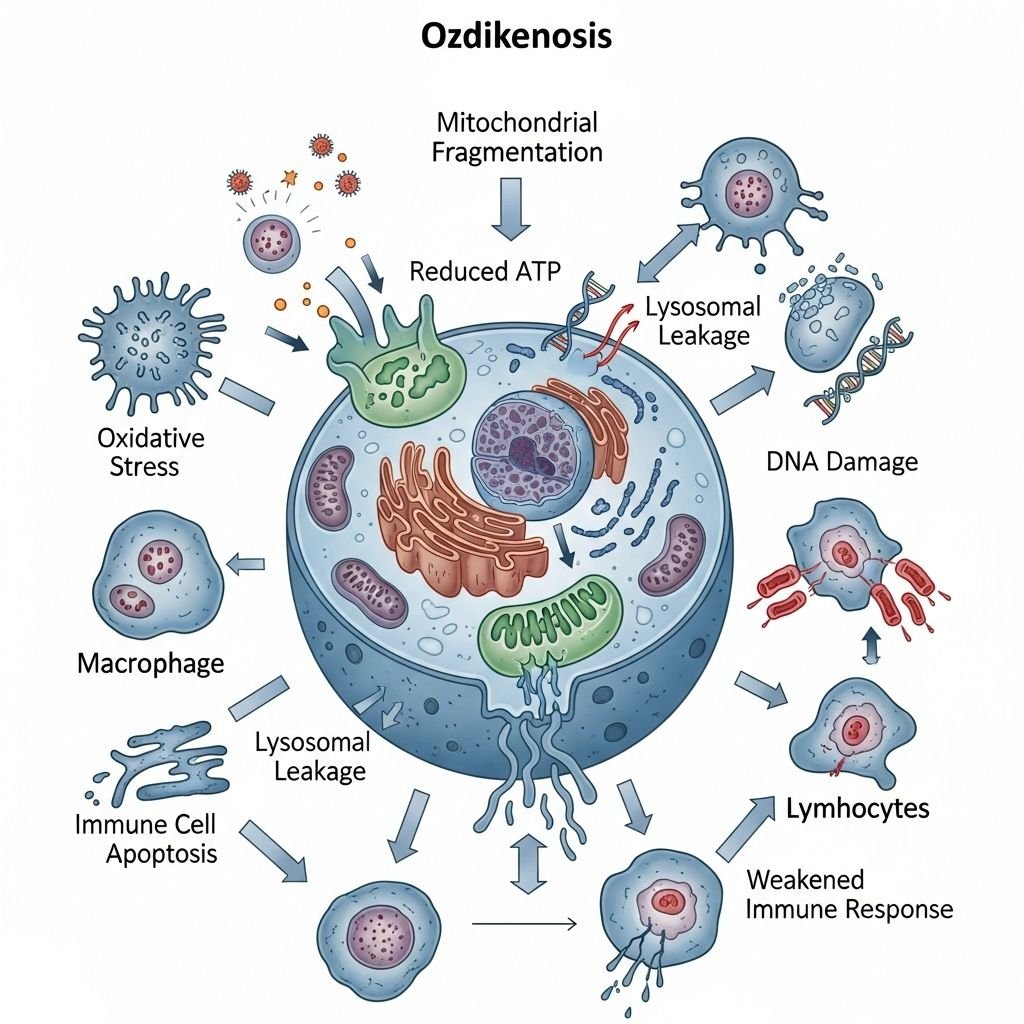
The disease essentially shuts down the body’s energy production and defense mechanisms.
Core Mechanisms of Cellular and Metabolic Breakdown
At its core, Ozdikenosis is a metabolic disorder. It primarily affects the mitochondria, the tiny “powerhouses” within our cells responsible for creating energy (ATP). The disease causes these mitochondria to malfunction, leading to a state of cellular exhaustion. Without sufficient energy, cells begin to die, leading to tissue damage and widespread inflammation.
The Progression of Organ System Failure
As the cellular energy crisis spreads, the organs that require the most energy are the first to suffer. The body’s systems progressively fail one by one.
- Neurological Degeneration: The brain, which consumes a high percentage of the body’s energy, is severely impacted. Patients may experience cognitive decline, memory loss, seizures, and a loss of motor control.
- Cardiovascular and Respiratory Damage: The heart muscle weakens, leading to an irregular heartbeat and, eventually, heart failure. The diaphragm and other respiratory muscles weaken, causing breathing difficulties and, ultimately, respiratory failure.
- Liver and Kidney Dysfunction: The liver and kidneys, which are essential for detoxification, lose their ability to filter waste. This leads to a toxic buildup in the bloodstream and severe metabolic imbalances that are life-threatening.
Symptoms and Diagnosis of Ozdikenosis
Because its early symptoms are often vague and can mimic other common conditions, Ozdikenosis frequently goes undiagnosed for years.
Recognizing the Early Symptoms of Ozdikenosis
Early signs typically include chronic fatigue, muscle weakness, and a general feeling of malaise. As the disease progresses, more specific symptoms may emerge, such as joint and organ pain, increased susceptibility to infections, and unexplained fevers. A key red flag is a combination of these symptoms that worsen over time without a clear cause.
| Symptom Category | Common Symptoms | Prevalence |
| Metabolic | Chronic fatigue, weight loss, muscle weakness | Very High |
| Neurological | Memory loss, tremors, seizures | High |
| Immunological | Recurrent fevers, frequent infections | High |
| Cardiovascular | Irregular heartbeat, shortness of breath | Moderate |
The Diagnostic Process: How Do You Test for Ozdikenosis?
Diagnosis is a challenging process that often involves a “diagnostic odyssey.” Doctors typically begin by ruling out more common diseases before they order a test for Ozdikenosis. A definitive diagnosis is usually reached through a combination of:
- Genetic Testing: Identifying the specific mutation in the genes responsible for cellular metabolism.
- Metabolic Screening: Blood and urine tests to detect the presence of toxins and imbalances caused by the failing organs.
- Medical Imaging: Scans like MRIs and CTs to check for signs of organ damage and neural degeneration.
The Stages of Ozdikenosis
Ozdikenosis is a progressive disease that unfolds in three distinct stages, each marked by an escalation of symptoms and an increase in severity.
- Stage 1: Initial Metabolic Changes: This early phase can last for months or even years. Symptoms are subtle and often dismissed as fatigue or stress. The body’s cells begin to experience minor energy deficits, but organ function is largely preserved.
- Stage 2: Progressive Organ Function Decline: During this stage, which typically occurs within the first year of severe symptoms, organ systems begin to show noticeable decline. Patients experience more severe symptoms, such as consistent muscle pain and cognitive difficulties. Organ function may drop by 15-20%.
- Stage 3: Multiple Organ Failure: The final stage is marked by a rapid and catastrophic breakdown of multiple vital systems. Organ function falls below 50%, leading to severe complications like respiratory distress, seizures, and cardiac arrest. Survival is typically measured in weeks or months at this point.
Ozdikenosis Treatment and Management
Currently, there is no known cure for Ozdikenosis. Treatment is therefore focused on managing symptoms and providing supportive care to slow the disease’s progression and improve the patient’s quality of life.
Why Can’t Ozdikenosis Be Cured?
The primary reason a cure remains elusive is the disease’s genetic origin. Ozdikenosis is not an infection or an injury but a systemic flaw in the body’s fundamental genetic code. Current medical tools can treat the symptoms of organ failure, but they cannot fix the underlying genetic mutation that is causing the problem.
Current Treatment Options and Supportive Care
Treatment is highly personalized and multidisciplinary. It may include:
- Metabolic Supplements: Doctors may prescribe specialized vitamins and coenzymes to help improve cellular energy production.
- Symptomatic Medications: Drugs are used to manage specific symptoms, such as anti-inflammatories for pain, anti-convulsants for seizures, and cardiac medications to support heart function.
- Supportive Care: This includes physical therapy to maintain muscle strength, nutritional support to ease the metabolic burden, and psychological counseling to help patients and families cope with the diagnosis.
Future Outlook: Research and Promising Therapies
The hope for a cure lies in emerging fields of medicine that can address the disease’s genetic root.
The Role of Gene Therapy and Stem Cells
Researchers are exploring therapies that could potentially correct the genetic mutation or replace damaged cells. Gene therapy introduces a healthy copy of a defective gene to restore a cell’s normal function. Stem cell treatments, on the other hand, aim to replace damaged or failing cells with healthy ones. While these therapies show promise in labs, they are still in early-stage trials and face significant safety and ethical hurdles.
| Treatment Approach | Success Rate (in trials) | Average Survival Extension |
| Symptomatic Management | 70% (of symptom relief) | 12-18 months |
| Immune System Modulators | 45% (slowed progression) | 18-24 months |
| Experimental Gene Therapy | 15% (partial cellular repair) | 36+ months |
Final Thoughts
Ozdikenosis is a heartbreaking condition that poses immense challenges for patients and their families. However, with growing awareness and an accelerating pace of research, there is increasing hope for better treatments and, one day, a cure. The ongoing work in genetic and regenerative medicine is paving the way for a future where a diagnosis of Ozdikenosis may not be a fatal verdict.
Disclaimer
This article is for general informational purposes only and is not medical advice. For a proper diagnosis and treatment plan, please consult with a qualified healthcare professional.
FAQs
Is Ozdikenosis contagious?
No, Ozdikenosis is a genetic disorder. It is inherited and cannot be passed from person to person through contact or other means.
Can a person with Ozdikenosis live a normal life?
In its early stages, a person may experience relatively mild symptoms and maintain a good quality of life with proper management. However, as the disease progresses, it becomes life-limiting and requires extensive care.
Why is it so hard to get a diagnosis?
The early symptoms of Ozdikenosis are very general and often mimic other conditions like chronic fatigue syndrome or fibromyalgia, which can lead to a lengthy “diagnostic odyssey.”
Is Ozdikenosis an autoimmune disease?
While Ozdikenosis can trigger an immune system response that damages healthy tissue, its root cause is a genetic malfunction, not a primary autoimmune disorder.